Latest in Health & Science News
Get up-to-date health & science news from our reporters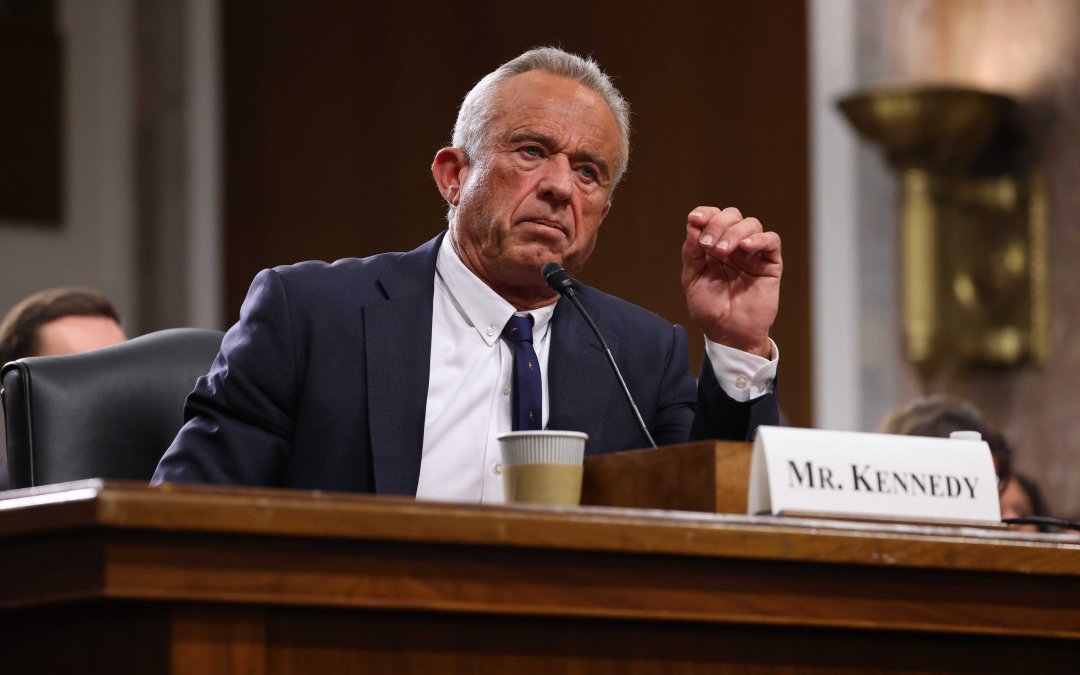
Watch: Past comments on vaccines and abortion dominate RFK Jr. confirmation hearing
Kennedy’s prior statements on vaccine efficacy have raised concern among Democrats.
read more
RFK Jr. dodges questions on Medicaid, vaccines at confirmation hearing
The Senate Finance Committee interrogated Trump’s nominee for Secretary of Health and Human Services Wednesday.
read more
Democrats warn: Veterans will suffer from Trump’s federal funding freeze
Members of the Senate Veterans’ Affair Committee aired frustrations over the potential ramifications to veterans care in a committee hearing Tuesday, after President Donald Trump’s sweeping order to freeze federal funding.
read more
Committee members come together to discuss topic that affects all: Aging.
The Senate Special Committee on Aging discussed promoting wellness among older Americans.
read more
Trump’s Energy Secretary nominee says the solution to climate change is a more evolved energy system
Chris Wright said he believes in climate change and has followed its evolution for more than two decades.
read morePandemic telehealth rules expanded access to lifesaving addiction medication. Will the next DEA leader extend the flexibilities?
The medication buprenorphine, used by patients with opioid use disorder (OUD), became easier for Americans to access in 2020 as a result of the COVID-19 pandemic. However, this access is only a temporary protection, and experts say the clock is ticking before thousands of patients lose access in 2025.
Buprenorphine, often referred to by the brand name Suboxone, is a partial opioid agonist, meaning it helps people with opiate use disorder quit using opioids by reducing cravings and lessening withdrawal symptoms. It is the only medication of its kind that primary care providers can prescribe. Before the pandemic, patients needed to be evaluated in person by a prescriber before they could start taking buprenorphine. During the COVID public health emergency, the in-person requirement was lifted, allowing providers to prescribe the medication via telehealth.
Lauren Majors, a nurse practitioner and addiction nurse practitioner program manager at Boston’s Beth Israel Deaconess Medical Center, said the ability to prescribe Suboxone online has significantly expanded the number of patients who can access treatment.
“It’s huge,” Majors said. “I was actually just talking to a patient today who lost his license due to substance use, and so getting to appointments can be incredibly challenging for patients. Many of them don’t have licenses or can’t drive, and so just by offering it, you’re reaching a broader audience.”
In 2020, an estimated 2.7 million people in the United States aged 12 and older had an OUD in the past 12 months, according to the National Institute on Drug Abuse. The opioid crisis has remained a significant issue across the country, with 107,941 people dying of an overdose in 2022, according to NIDA.
Between April 2023 and April 2024, overdose deaths declined by roughly 10 percent, according to the Centers for Disease Control, making it the largest decrease on record. The exact reason for the decline is unknown, but greater access to buprenorphine could be a contributing factor.
To prescribe Suboxone, a controlled substance, providers must obtain a U.S. Drug Enforcement Agency License by answering questions, paying a fee and waiting for their application to be processed. Rural areas may lack a nearby provider with a DEA license, so the pandemic flexibilities for Suboxone have been instrumental in allowing patients to access the medication, especially since some prescribers don’t have in-person appointments available for weeks.
Marcelo H. Fernández-Viña, who researches access to substance use treatment for Pew Research Center, said more patients than ever have been able to start and stay in treatment for OUD without an increase in overdose rates.
“Veterans, people experiencing homelessness, people that were involved in the criminal justice system, people living in rural areas, racial and ethnic minorities-they all got greater access to buprenorphine via telehealth,” Fernández-Viña said. “It really helped with barriers like transportation or finding childcare or taking time off work. And the research also showed that patients liked it and that providers liked it, too.”
But these pandemic flexibilities aren’t permanent. In March 2023, the U.S. was no longer in a state of public health emergency, so the DEA proposed changing the rules. Under the proposal, patients would have been able to get one 30-day supply of buprenorphine before having to visit their provider in person for another prescription. The DEA received over 38,000 comments in response to the proposed changes to telemedicine, with the vast majority advocating for a continuation of entirely online care.
As a result, the DEA extended the flexibilities through November 2023, and then again through December 2024. The most recent extension provides an additional year of buprenorphine access via telehealth, through the end of 2025.
Fernández-Viña said the temporary nature of these rules has made the future of OUD care uncertain for both patients and providers.
“It has left many providers hesitant to invest in telehealth services, and it leaves patients continually in danger of losing access to this treatment,” he said. “People don’t know what their treatment is going to look like after these things expire.”
With the new presidential term beginning in 2025, patients remain unsure what will happen to their Suboxone access. Extending telehealth rules takes time, as the DEA is required to offer a public comment period of 30 or 60 days before reviewing responses, addressing major concerns and finalizing the extension.
“That’s a long process. It’s a lot of bureaucracy. So that takes time,” Fernández-Viña said. “In addition to that, it’s a new administration, there’s new folks. Getting people up and running takes time, so a year is tight.”
Congress also can make these telehealth provisions permanent. The Telehealth Response for E-prescribing Addiction Therapy Services (TREATS) Act was proposed in the Senate in November 2023, but it has yet to see any legislative progress. Both Congress and the DEA feel the other should oversee the policy change.
Sen. Mike Braun (R-Ind.), who serves on the Senate Health, Education, Labor and Pensions (HELP) Committee, said he favors keeping the flexibilities in place, and views it as a worthy legislative pursuit. “I love telehealth. I think you should be able to do anything through telehealth because it’s generally going to be a lower cost when it comes to that, or almost anything else in health care.”
When asked why Congress has not acted on the issue, Braun said that “the health care industry isn’t that interested in it, as they should be, because it would probably lower their revenues.”
Sen. Tim Kaine (D-Va.), another HELP Committee member, said he intends to look into the safety of buprenorphine. “I don’t have yet a conclusion about that,” he said. “It would be a mistake just to go back to where we were before. Exactly how the telehealth prescription of buprenorphine has worked, and has it been a good thing with no unintended downsides or consequences, I don’t really know. I’d want to take a look at it, but I do generally think that our use of telehealth during the COVID was one of the real smart things we did.”
President-elect Trump tapped Chad Chronister, a Florida sheriff, for DEA Administrator, but Chronister withdrew his name for consideration earlier this month. Trump later took to Truth Social, saying that Chronister did not withdraw his name but instead, pulled his support for the sheriff. A replacement has yet to be named, but lawmakers, providers and patients remain unsure how the new executive branch will proceed.
Kyle Zebley, Executive Director of ATA Action, a group affiliated with the American Telemedicine Association that advocates for the expansion of telemedicine services, noted that Congress originally granted the DEA the ability to allow providers to prescribe controlled substances without an initial in-person visit in 2008. Yet, 16 years later, a permanent solution remains elusive.
“I think that the new administration will want to take a look at what the outgoing Biden administration has done in terms of their draft rule, which is not publicly available yet, and see if they will want to continue with it or change course,” Zebley said. “I think that they will likely want to change course and put their own imprint on it. That takes time.”
The main hesitancy surrounding expanding Suboxone access is a practice called diversion—the illegal distribution of medication from a patient with a prescription to someone without one. But Fernández-Viña said that studies have proven the best way to prevent diversion is to increase access, which the pandemic flexibilities have done in a major way.
“We’ve got this one year, and then once that year is up, if nothing gets done, then people lose access,” Fernández-Viña said. “We’re really heading towards the cliff.”
Supreme Court appears to side with state’s ban on transgender youth treatments
WASHINGTON — Conservative Supreme Court justices raised doubts about the challenge to Tennessee’s ban on gender-affirming medical care for transgender minors during oral arguments for United States v. Skrmetti Wednesday.
Enacted in 2023, Tennessee’s Senate Bill 1 bars health care providers from prescribing puberty blockers and hormone therapy to minors with gender dysphoria, even with parental consent. The condition causes distress even with parental consent. The condition causes distress because of a mismatch between their biological sex and their gender identity.
Advocacy groups, including the ACLU and Lambda Legal, challenged the law on behalf of affected families, such as Nashville parents Samantha and Brian Williams and their transgender daughter.
Solicitor General Elizabeth Prelogar, representing the challengers, argued that Tennessee’s blanket ban is both overbroad and harmful, failing to account for health risks tied to untreated gender dysphoria, such as elevated suicide rates among transgender youth.
“Rather than impose measured guardrails, SB1 bans the care outright no matter how critical it is for an individual patient, and that approach is a stark departure from the State’s regulation of pediatric care in all other contexts,” Prelogar said.
Hundreds rally as Supreme Court hears case on gender-affirming care for transgender youth (Emma Richman/MNS)
West Virginia, which requires procedural steps including a psychological evaluation to receive medications for gender dysphoria, was cited as an alternative to the law.
Chief Justice John Roberts rigorously questioned Prelogar asking whether the court should leave health care regulations to state legislative bodies.
“The Constitution leaves that question to the people’s representatives rather than to nine people, none of whom is a doctor,” Roberts said.
Other justices echoed similar concerns, including Justices Clarence Thomas and Brett Kavanaugh.
Justice Kavanaugh also voiced concerns about the medical risks posed to transgender youth, pointing out that some European countries’ research revealed concerns about the effects of hormone therapy on transgender youth.
“If it’s evolving like that and changing and England’s pulling back and Sweden’s pulling back, it strikes me as a pretty heavy yellow light, if not red light, for this court,” Kavanaugh said.
Justice Samuel Alito echoed a similar sentiment, citing Swedish data that appeared to be contrary to the solicitor’s claims that the treatment is more beneficial than risky.
Prelogar pushed back, citing both that Tennessee has not “substantiated those risks” in court and despite those research findings, European countries have not categorically banned medication for transgender youth.
“There has been no change in the law that I’m aware of in Sweden, Finland and Norway. Each of the medical authorities in those states has called for an individualized approach to care,” Pelogar said. “But they have not changed their laws to do anything like what Tennessee is doing here.”
William Eskridge, a Yale law professor who wrote an amicus brief opposing SB1, told the Medill New Service that the WPATH standards of care, transgender therapy guidelines, is approved by the American Medical Association.
“The medical consensus is still in favor of very cautious, medically supervised treatments for adolescents who have serious gender dysphoria,” William Eskridge said, a Yale law professor who wrote an amicus brief opposing SB1. “Name me one significant medical procedure that does not have risks and side effects.”
Matthew Rice, Tennessee’s solicitor general, defended the law by asserting that its focus is on medical intent rather than a patient’s sex, and that the law’s wording, “Inconsistent with sex” was solely used to “describe a single prohibited medical purpose.”
He argued that the measure was designed to protect minors from risk-heavy medical treatments that could have “irreversible and life-altering consequences.” Therefore, the law was not intentionally discriminatory based on sex.
“Just as using morphine to manage pain differs from using it to assist suicide, using hormones and puberty blockers to address a physical condition is far different from using it to address psychological distress associated with one’s body,” Rice said.
The law blocks minors from accessing gender-affirming treatments while still permitting the same medications to be used for other conditions for cisgender youth, such as early-onset puberty. This inconsistency forms part of the critique against the law, which opponents argue is vague and grounded in outdated gender stereotypes.
Yale Law Professor Issa Kohler-Hausman, who co-authored an amicus brief with Yale philosophers and lawyers, described Tennessee’s defense as deeply flawed. Despite the defense’s argument that medications are risky for transgender youth, she said the law aims to enforce gender norms, with SB1 encouraging minors to “appreciate their sex.”
“[Tennessee’s] argument is literally incoherent unless, you’re already packing in social expectations and roles and cultural assumptions into the word ‘sex’, because what the Republican justices and conservative legal activists want to always do, is pretend that they’re using sex in this a purely biological way,” Kohler-Hausman said. “That’s nonsense.”
Justice Sonia Sotomayor pushed back against the state’s argument, noting the high rates of suicide among minors with gender dysphoria.
“One of the Petitioners in this case described throwing up every day, going almost mute because of their inability to speak in a voice that they could live with,” Sotomayor said.
Justice Ketanji Brown Jackson also expressed concern about the court siding with Tennessee, noting that similar reasoning was once used to defend state bans on interracial marriage, which the Supreme Court struck down in 1967.
Jackson cautioned that doing so could erode the principles underpinning key equal protection rulings, questioning whether the court risked weakening its foundational precedents.
“A law is drawing lines on the basis of some suspect classification,” Jackson said.
The Court is expected to release a decision this summer.
Lawmakers spar with NIH director over vaccine rhetoric, racial equity
WASHINGTON – Lawmakers sparred with Dr. Monica Bertagnolli, Director of the National Institutes of Health (NIH), over vaccines and the future of the agency under President-Elect Donald Trump at a House Appropriations Committee Hearing on Tuesday.
The hearing was held just days after Trump tapped former presidential candidate Robert F. Kennedy Jr. to lead the Department of Health and Human Services, which oversees the NIH. Kennedy, a vocal vaccine skeptic, has called for an overhaul of HHS’s agencies, claiming that federal agencies are allied with food and drug companies that are worsening the health of Americans. Rep. Andy Harris (R-Md.) said he had spoken to Kennedy about his plans for the department.
“America’s getting sicker and not healthier,” Harris said. “There’s a reason why Mr. Kennedy and Mr. Musk are going to have a study in this, because I think they realize that we have to make America healthy again.”
Harris pressed Bertagnolli on the NIH’s study of nutrition-related diseases in the U.S. He cited a phone call to the NIH’s Office of Nutrition Research during which he claims his staff was informed that the agency does not have a scientist specializing in nutrition-related diseases.
“Obesity, hypertension, diabetes-these are the drivers of huge costs in our Medicare program,” Harris said. “Do you really not have a scientist at NIH who specializes in studying diet-related disease?”
“That perception could not possibly be more wrong,” Bertagnolli said in response. “I can’t think of a single institute or center across NIH that doesn’t, in some way or form, have research that touches on nutrition.”
Later in the hearing, Harris questioned the NIH’s biological research involving transgender individuals, asking Bertagnolli whether the agency would report a transgender woman as a biological male or female.
“We assign them according to the biological research question we are trying to answer,” Bertagnolli said. “We’re not going to say they’re a man or they’re a woman. We are going to base it off the science and the scientific question we’re trying to answer.”
“And that’s why nobody trusts the NIH,” Harris responded.
The Appropriations Committee, which oversees federal discretionary funding, discussed the President’s Budget for Fiscal Year 2025. The budget requests a $1.2 billion increase in federal funding for the NIH, which plans to boost funding for women’s health and vaccine development.
Rep. Lois Frankel (D-Fla.) expressed concern about anti-vaccine rhetoric among members of the incoming administration, seemingly critical of Kennedy, and asked Bertagnolli about the risks of not vaccinating children in the U.S.
“If all vaccination suddenly stops, we will see much more severe illness and death in children,” Bertagnolli said. “There are other places in the world that have this, that do not have widespread vaccination of their populations, and look at the tragedies that we see there. I think it would be very disturbing.”
Bertagnolli was also pressed by Rep. Andrew Clyde (R-Ga.) on a “deeply concerning” 2023 investigation into NIH officials’ use of personal email accounts to evade the Freedom of Information Act.
Bertagnolli refused to comment on ongoing personnel matters within the agency, but Clyde persisted. “Congress is an investigative body. We are doing an investigation here,” he said. When I ask you a question, I need a response.”
Bertagnolli promised that she would look into the matter and that the NIH will abide by all legal requirements, including preserving records and being transparent with the incoming Trump administration.
She also cited the NIH’s study of gene therapies for rare diseases, which the for-profit sector is unlikely to invest in, as a way to make health care more accessible. Once the NIH develops effective treatments, the agency can sell the therapies to the private sector under strict regulations to keep therapies affordable for Americans.
“We have a researcher who is doing in-utero gene therapies. Wouldn’t that be wonderful if we could test a baby even before it’s born, deliver a treatment and eliminate suffering from things like this?” Bertagnolli said. “NIH needs to take even these very rare diseases under our wing and really champion the gene therapies that can be ideally curative for these individuals.”
Why voters chose to protect abortion and vote for Donald Trump, according to experts
WASHINGTON– Experts say the successful protection of abortion rights in seven states Tuesday shows reproductive rights are popular among voters. However, an interesting scenario in four states is raising questions about the issue.
Voters in Nevada, Arizona, Montana and Missouri voted for both state amendments to protect reproductive rights and former President Donald Trump, helping him win the 2024 presidential election.
The former President has taken credit for the fall of Roe v. Wade in 2022, removing federal protections for abortion rights. Trump nominated three justices to the Supreme Court, all of whom voted to overturn the 1973 decision in the case Dobbs vs. Jackson Women’s Health Organization.
The two outcomes represented a stark “dissonance” among voters, according to Melissa Goodman, Executive Director of the UCLA Center on Reproductive Health, Law and Policy. She said that voters simultaneously voted to protect and harm those rights.
“We have these overwhelming wins in ballot measures to protect abortion rights around the nation and a majority of voters obviously elected Donald Trump, which will unquestionably have extremely devastating consequences for reproductive health care access and gender equality in our country for the next four years,” Goodman said.
Exit polling shows abortion was not the most important thing on voters minds in the voting booth. According to a Washington Post report, 66% of voters felt the economy and “the state of democracy” were the most important issues. On abortion, polling found just 14% of voters had reproductive rights as their top issue.
Goodman contends that a big reason for the lesser concern and disconnected results was that Donald Trump effectively “obfuscated” his own views and policies on the issue. She points to the former president’s repeated commitment to leave things to the states and at times murky view on signing a national abortion ban.
“In these states where they had the ability to kind of express their views about abortion in the way of a state ballot measure, that was the way they expressed their feelings on that subject, and then possibly felt free to express their opinion on other topics in their candidate votes,” Goodman says.
Long-time Democratic party pollster Celinda Lake agrees. She said the state amendments “almost gave [voters] permission” to vote on their other concerns by making it “impossible for [politicians] to act further on the abortion issue.”
Lake said that Vice President Kamala Harris did a “brilliant job on the abortion issue,” and that her loss was not a failure in her messaging on reproductive rights. She said the results of the election and abortion amendments shows Harris fell short in her messaging about the economy, something Lake says is a long-time issue in Democratic platforms. But the issue in Lake’s eyes isn’t the quality of the policy, but trouble with getting the word out about them.
According to Lake, she found through focus groups that 60% of people don’t really know what Democrats stand for economically, and that lack of clarity may have impacted voters when deciding who to give the economic reins to for the next four years.
“We don’t have an economic brand, and we start out every campaign 20 points behind on the economy,” Lake says. “We have to step back and have an economic brand that works for working people.”
Goodman and Lake both said that pollsters, strategists and academics will have to work to find out what happened this election, and understand how abortion was outshone by other concerns.
But they agree the takeaway here should not be that abortion does not matter to voters.
“There remains extremely strong support for abortion rights throughout this country, despite the actual presidential election result,” Goodman said.
NASA’s Parker Solar Probe Completes Final Venus Flyby
WASHINGTON – NASA’s Parker Solar Probe executed its final gravity-assist maneuver on Wednesday, flying past the surface of Venus and setting it on a path to come within 3.86 million miles of the solar surface, the closest any human-made object has ever come to the sun.
The probe used gravitational pull to alter its trajectory, coming within 233 miles of the surface of Venus, according to a NASA press release. Parker has now completed seven flybys of Venus in preparation for its approach to the sun, which will occur on Dec. 24, 2024.
“The physics of how the energy from the sun turns into space weather, which affects the earth, is not well understood,” said Dr. James Lattis, professor of astronomy at the University of Wisconsin-Madison and Director of the UW Space Place. The probe’s solar approach will be instrumental in understanding space weather, or conditions in the portion of space closest to Earth’s surface, which includes magnetic fields and particles that affect the earth.
“The main goal of this probe is to improve our understanding of that very important physics,” Lattis said.
NASA launched the Parker Solar Probe in 2018 in order to garner more data about the sun’s outermost layer, called its corona, and the magnetic processes that occur on the solar surface. Entering Venus’ gravity is critical to the mission in order to slow the probe’s trajectory prior to its solar approach, during which it will come within an unprecedented 3.86 million miles of the solar surface, according to NASA.
Additionally, images taken during the flyby will contribute to NASA’s knowledge of the conditions on Venus’ surface. The Wide-Field Imager for Parker Solar Probe (WISPR) is the imaging instrument on the Parker Probe, and during previous Venus assist maneuvers, WISPR captured images of Venus’ surface below its thick cloud cover.
“This is an unexpected bonus science,” said Dr. Adam Szabo, chief of the Heliospheric Physics Laboratory at NASA. “Parker Solar Probe was not designed to do planetary science, but since we are flying next to Venus, we started to assess ‘well, what can we do to look at the planet?’”
In 1989, NASA launched the Magellan spacecraft, which studied the topography of Venus. Szabo noted that the more current images taken by WISPR showed possible physical and chemical changes to Venus’s surface since the Magellan mission. Wednesday’s final gravity assist maneuver will provide additional information regarding these potential changes.
“We’re actually able to compare what changes have happened over time. We don’t really understand the geology of Venus that well, so it’s an opportunity to see how things have changed, and try to think about why it’s changed in the years since Magellan,” said Dr. Veronica Dike, a post-doctoral research associate at the University of Illinois.
Astronomists look forward to the probe’s findings following its Dec. 24 approach, especially since there is still so much to learn about how the sun functions.
“The big takeaway with this flyby of Venus is that we are going to get closer than humanity has ever gotten to a star before,” Dike said. “I think it’s a big engineering achievement that we built something that can get as close as the Parker Solar Probe will.”
What states will have abortion on the ballot this year?
WASHINGTON – Abortion will be on the ballot in 10 U.S. states this Tuesday as voters turn out for the first presidential election since the Supreme Court overturned Roe v. Wade in 2022.
Almost all of the ballot measures aim to enshrine the right to abortion, including the referendum in South Dakota, where reproductive rights advocates seek to end the state’s total abortion ban.
Abortion access has been a focal point of the 2024 presidential election and will play a key role in mobilizing voters. David Cohen, Professor of Law at Drexel University’s Thomas R. Klein School of Law and one of the leading national experts on abortion, said that this election year is hugely important in the history of abortion access in the U.S.
“It’s irrelevant what happens on these state ballot initiatives if Donald Trump wins,” Drexel said. “Even if a state protects abortion, if the federal government bans it, or makes it extremely difficult, that trumps state law, even if a state has passed a constitutional amendment protecting it.”
The citizen-initiated ballot measures required months of canvassing by abortion advocacy groups in order to reach the signature threshold, and both pro-life and pro-choice organizations have been busy encouraging voters to head to the polls.
Chris Melody Fields Figuerdo, executive director of Ballot Initiative Strategy Center, a liberal advocacy organization, feels confident that voters will opt to protect reproductive rights regardless of political affiliation.
“Republicans, Democrats and Independents in states like Kansas and Kentucky, where the electorate may seem more conservative, voted against those abortion bans,” Figuerdo said. “We do know that the issue of abortion and reproductive rights is a highly motivating issue for voters.”
Since 2022, seven states thus far have had abortion on the ballot, with all seven choosing to vote in favor of abortion rights.
Arizona
Arizona’s Right to Abortion Initiative would establish the right to abortion until the point of fetal viability, usually considered around 24 weeks.
Colorado
The Right to Abortion Initiative in Colorado would enshrine the right to abortion in the state’s constitution and allow public funds to be used for abortion.
Florida
Florida Amendment 4 seeks to expand abortion rights in the state by allowing for the procedure until fetal viability or when deemed necessary to protect the health of the patient.
Maryland
Maryland’s Right to Reproductive Freedom Amendment would enshrine the right to an abortion in the state constitution, establishing a right to “reproductive freedom,” including decisions to prevent, continue or end one’s own pregnancy.”
Missouri
The Right to Reproductive Freedom Amendment in Missouri would establish the right to reproductive freedom in the Missouri Constitution and only allow the state’s legislature to pass laws regulating abortion after the point of fetal viability.
Montana
Montana’s CI-128, Right to Abortion Initiative, seeks to amend the state constitution to allow for the right to an abortion, a right which is already held in the state.
Nebraska
Nebraska has two ballot measures. The Prohibit Abortions After the First Trimester Amendment would prohibit abortion in the second and third trimesters. The Right to Abortion Initiative would allow citizens to obtain an abortion until fetal viability, an expansion of rights from the currently-enforced 12-week
New York
The Equal Protection of Law Amendment would add language to the New York Bill of Rights that people cannot be denied rights based on "sexual orientation, gender identity, gender expression, pregnancy, pregnancy outcomes, and reproductive healthcare and autonomy."
Nevada
Nevada’s Right to Abortion Initiative seeks to allow for the right to an abortion until fetal viability in the state’s constitution.
South Dakota
South Dakota’s Constitutional Amendment G would provide a trimester framework for regulating abortion in the State Constitution, which would include the right to an abortion for all citizens during the first trimester of pregnancy.
Point by Point – Episode 3: Costs vs. Access – The Diverging Health Care Paths of Trump and Harris
In this third episode of Point by Point, we focus on health care by comparing former President Trump’s efforts to repeal the Affordable Care Act with Vice President Kamala Harris’s commitment to expanding health care access. Tune in as we explore how their policies on health care costs, insurance coverage, and prescription drug prices could shape the future of the U.S. health care system.
Listen here:
Health care professionals call on Trump to release medical records
WASHINGTON – More than 200 doctors and nurses are calling on former President Donald Trump to release his medical records, citing concerns over his age and fitness for office as he campaigns for a potential second term that would make the 78-year-old the oldest president-elect in history.
So far, Trump has resisted their pressure.
Dr. Ezekiel Tayler, a critical-care physician from Pennsylvania, was among the 238 signatories of a letter from Doctors for Harris, an independent grassroots organization that is not affiliated with the Harris-Walz campaign. He said he signed the letter because he believes anyone running for America’s highest office has a responsibility to be upfront with voters.
“I think what Donald Trump has done is normalize a lack of transparency, saying: ‘I can do whatever I want, whenever I want to do it, and if you don’t like it, well, I am who I am’ and that’s not appropriate,” Tayler said.
The letter, which was dated Oct. 13, noted that without a disclosure of health data, doctors and voters are forced to draw conclusions from Trump’s behavior during public appearances. They said that in that regard, “Trump is falling concerningly short of any standard of fitness for office and displaying alarming characteristics of declining acuity.”
Trump’s history of health disclosure controversy
When Hillary Clinton’s campaign published her detailed medical report over a year before the 2016 election, Trump faced pressure to follow suit.
In a December 2015 tweet, he said he’d release a full medical report that would “show perfection.”
Ten days later, his personal doctor issued a four-paragraph letter that included no specific health statistics, but claimed that Trump “will be the healthiest individual ever elected to the presidency.” It was later revealed that Trump had dictated this letter and his doctor simply signed it.
In 2020, Trump tested positive for COVID-19 after Justice Amy Coney Barrett’s Supreme Court confirmation on September 26 but waited until October 2—three days after a presidential debate with Joe Biden—to announce it. This detail came to light a year later after Trump’s former chief of staff, Mark Meadows, published it in his 2021 book.
Health concerns grow ahead of the election
Now, in lieu of publishing an updated medical report, as Trump promised he would do in an August 2024 interview, his campaign issued a statement citing two July memos from former White House physician and current Texas congressman Dr. Ronny Jackson, who treated the former president after he was shot in an assassination attempt this summer, as proof that Trump is fit for office.
“I want to receive a solid health report, not from the doctor who examined him last time—who had his own issues—but from a respected physician, so I can comprehend what is happening with him,” said Pat Ford-Roegner, a nurse practitioner and member of Nurses for America, a group that started working with Doctors for Harris earlier this year.
Ford-Roegner said that she believed the “level of anger” Trump is displaying in his recent public appearances is the most alarming aspect of his behavior. The Doctors for Harris letter cited similar worries.
“As we age, we lose our sharpness and return to basic instincts. We are witnessing this with Trump, as he utilizes his rallies and appearances to ramble, meander, and crudely lash out at his numerous perceived grievances,” the doctors wrote. They pointed to his recent claim that Haitian immigrants are eating pets in Ohio as a specific example.
In the week after the letter, Trump took the stage at a town hall in Pennsylvania, where he danced and swayed to his personal playlist for nearly 40 minutes after abruptly ending the Q&A portion of the event. Dr. Mark Lopatin, a retired rheumatologist who also signed the letter, highlighted this as another cause for concern.
“The public deserves to know what’s going on,” Lopatin said. “So I think anytime someone is not being transparent we should call that out.”
FDA and NIH discuss smoking cessation practices, reviving e-cigarette debate
WASHINGTON –The Food and Drug Administration and National Institutes of Health analyzed practices for reducing tobacco consumption, including switching from traditional cigarette use to e-cigarettes, at a joint public meeting on smoking cessation on Monday.
“We’ve made real progress in reducing cigarette smoking in the U.S., which is a notable public health achievement,” said FDA Commissioner Dr. Robert Califf. “While this progress is encouraging, we still have much more work to do, including addressing disparities in the types of products being used and who is using them.”
The meeting’s topics ranged from medications like Bupropion and Varenicline, which help people quit by reducing nicotine withdrawal symptoms, to new apps designed to coach people through smoking cessation.
The nation’s top tobacco cessation doctors also acknowledged that e-cigarettes are considered less harmful than standard cigarettes and could be a key pathway toward smoking cessation. But experts warn that vaping is not a risk-free alternative.
Vaping disperses toxic chemicals and heavy metals throughout the lungs, causing inflammatory injury and increasing risk for EVALI, or e-cigarette or vaping use-associated lung injury. Dr. Alejandra Ellison-Barnes, an assistant professor of general internal medicine at Johns Hopkins Hospital, works in a tobacco clinic, and says she encourages her clients to stop using tobacco products of any kind, including vapes.
“The important thing with e-cigarettes is that, because they’re relatively new, we don’t yet have a good body of evidence for the effects, both short term and long term,” Dr. Ellison-Barnes said. “It’s really a harm reduction and not a harm elimination strategy when you’re talking about e-cigarettes.”
Tobacco Industry and Campaigns
The smoking cessation meeting comes as e-cigarette use has been a recent campaign platform for presidential candidate Donald Trump, signaling what he may promote if elected. Trump vowed on Truth Social last month to “save vaping again” if elected, following a meeting with the Vaping Technology Association, a prominent vaping lobbyist.
Trump’s recent enthusiasm for vaping diverges from the stance of his previous administration, which raised the age requirement for purchasing e-cigarettes from 18 to 21 in 2019 and enacted a limited ban on fruit and mint flavored e-cigarettes in 2020. Both actions aimed to crack down on the widespread use of vapes among youth, since 1.63 million middle and high school students currently use e-cigarettes, according to CDC data.
The tobacco industry has backed Trump’s campaign, too. A subsidiary of the second leading tobacco company in the U.S. has donated $8.5 million to Make America Great Again Inc., the main super PAC for the Trump campaign, according to Open Secrets. The subsidiary, RAI Services Company, is the top corporate donor to the Trump-supporting super PAC. Vice President Kamala Harris’s campaign and the super PACs supporting it do not appear to have received donations from RAI Services Company.
“Cigarette smoking among adults has been cut in half since 2009, when the FDA gained the authority to regulate these products,” said Dr. Califf.
Yet smoking still kills nearly half a million U.S. residents each year, and financial support from the tobacco industry threatens to undo the progress that has already been made.
“I think any time there is industry money in politics, it’s a concern from a public health perspective,” Dr. Ellison-Barnes said. “Regardless of the administration, I think anytime there’s tobacco money mixed in, it’s definitely a public health concern.”
Disproportionate Impact
Smoking rates are concentrated in vulnerable populations like minority communities and those experiencing mental illness, and setbacks in smoking cessation could mean further disproportionate effects for these populations.
Dr. Lonnie Nelson, an associate professor at the Washington State University College of Nursing and a descendant of the Eastern Band of Cherokee Indians, spoke at Monday’s meeting. Dr. Nelson explained how the tobacco industry specifically targets Native Americans for consumption.
“American Indian and Alaska Native communities have the highest prevalence of commercial tobacco smoking of any racial or ethnic group in the U.S. We experience dramatic health disparities resulting from this fact,” Nelson said. “There is a need for efficacious and accessible interventions.”
An update on bird flu in the U.S.
WASHINGTON – A third case of bird flu was confirmed in California on Wednesday by the Centers for Disease Control and Prevention, following two other cases confirmed in the state last week. Two additional presumed cases are awaiting verification.
Wild birds, which are considered reservoirs for the virus, shed avian influenza and infect both poultry and dairy cows. According to CDC data, 295 herds of dairy cows have been infected, and 14 states have seen outbreaks in cattle. 100,781,821 poultry have been infected as of Oct. 8.
Humans who come in contact with these animals, especially dairy workers, are at risk of infection. This most recent case is the 17th instance of bird flu, a strain of influenza A known as H5N1, in the United States since March 2024.
The three known infected Californianians are dairy workers who were exposed to infected dairy cattle. Each case stemmed from a different farm, and patients reported mild symptoms. Typically, patients infected with the virus will experience respiratory symptoms, similar to the seasonal flu, or eye redness and irritation. But illness can range in severity from mild symptoms to severe symptoms that are fatal, according to the CDC.
There has been no evidence that the virus can spread between humans, but a patient in Missouri without known contact with animals was diagnosed with avian flu last month. One member of the patient’s household and six health care workers who came in contact with the patient subsequently developed symptoms of bird flu, the CDC said. The patient’s household member did not test for avian influenza, and one of the symptomatic health care workers tested negative, though the test was done after the ten-day testing window had elapsed.
Currently, experts are not concerned about human-to-human transmission. “At the present time, the risk to humans is really almost entirely limited to dairy workers,” said Dr. Dean Blumberg, Professor and Chief of Pediatric Infectious Diseases at UC Davis Health.
Blumberg says the concern lies in the risk of the virus mutating.“If the strains mutate, then there can be a risk of it mutating so there’s more human-to-human transmission. And then, instead of the infection risk being confined to the dairy workers, it could enter into the general population.”
So far, mutations have been limited. The Food and Drug Administration discussed avian influenza at its Meeting of the Vaccines and Related Biological Products Advisory Committee on Thursday.
Dr. Todd Davis, Acting Chief of the Virology, Surveillance, and Diagnosis Branch of the CDC, expressed optimism at the meeting. “These viruses thankfully have remained relatively genetically stable. We’re not seeing changes that impact increased infectivity or that would be predicted to yield increased transmissibility among people.”
Also discussed at the FDA Advisory Committee meeting was pandemic influenza preparedness and the progress that has been made on vaccine development.
Dr. Christine Oshansky spoke about the work of the Biomedical Advanced Research and Development Authority (BARDA) and its advanced production of vaccines for avian influenza. “We work with CDC and other WHO collaborating centers and we are monitoring the surveillance very closely of the animal viruses that are circulating around the world,” she said.
“I think it’s important for the FDA to be reviewing the avian influenza vaccines,” Dr. Blumberg said. “That’s a forward-thinking step. But at the present time, I think the major focus needs to be on surveillance of the dairy herds. We still have very little data about the prevalence of avian influenza within dairy herds, and part of that is because in most states, it’s voluntary for ranchers to allow their herds to be tested.”
Dr. Maurice Pitesky, Associate Professor at the UC Davis School of Veterinary Medicine-Cooperative Extension, expects that the virus is here to stay.
“It’s affecting so many different geographies and species that we’ve never detected it in before, and now we’re also finding it in human wastewater,” he said. “It’s the largest animal outbreak of disease we’ve ever had in the 5000 to 7000 years of domesticated agriculture. It’s significant, and it’ll probably continue to be that way.”
New Forever stamp honors health care workers
WASHINGTON — The United States Postal Service and the Department of Health and Human Services jointly launched a new Forever stamp honoring health care workers at a dedication ceremony on Thursday. The stamp became available for sale on Tuesday, October 1st and features the words “thank you” spelled out in various health-related icons. The words “healthcare community” run across the lower right corner of the stamp.
The health care community includes physicians, nurses, pharmacists, hospital custodians, lab technicians and epidemiologists, among others. USPS and HHS’s decision to honor health care workers comes in the wake of the Covid-19 pandemic, during which those in health care worked long hours taking care of those ill with the virus.
Xavier Becerra, secretary of the Department of HHS, spoke at Thursday’s ceremony. “Many of the first to die of Covid were in health care. And every day they do the job that we expect them to,” Becerra said.
Louis DeJoy, Postmaster General and Chief Executive Officer of the USPS, spoke of his interactions with health care workers throughout his own life. He expressed gratitude for the staff at the neighborhood clinic he and his siblings would visit as children, and he discussed the efforts of his wife Aldona, a physician who worked with AIDS patients at the beginning of the epidemic. This is DeJoy’s first stamp dedication in his four and a half years as postmaster general.
In January 2021, DeJoy and the USPS began working with the Administration for Strategic Preparedness and Response (ASPR), an agency within HHS, to distribute free Covid-19 test kits to Americans. Roughly 900 million test kits have been distributed thus far. The two organizations then decided to begin working on a Forever stamp to honor those working on the front lines caring for those sick with COVID-19.
“The members of the health care community, sometimes at great personal risk, have dedicated their lives to improving our health, safety and well being, and we owe them an enormous debt of gratitude for their service to the nation,” DeJoy said. “Health care workers have adjusted and still demonstrate acute awareness and the empathy necessary to provide not just medical care but emotional comfort to those they care for in their moments of great vulnerability. This embedded culture of kindness makes the world a better place.”
Remarks were also provided by Dr. Andrea Anderson, a family physician, associate professor, and the Associate Chief of Family Medicine at George Washington School of Medicine and Health Sciences. “Health care workers provided emergency health care when people could be saved and when they could not,” Anderson said. “There were faces shrouded behind masks and face shields breaking the bad news of a positive diagnosis to the terrified. There were those holding electronic tablets to allow a family member one last moment to say goodbye to a loved one, or they themselves became the last human voice heard when time had expired for yet another casualty of the microscopic virus less than the size of a human hair.”
Many health care workers became infected with Covid-19 during its peak, and the World Health Organization estimates that roughly 115,500 people in the health care community died between January 2020 and May 2021.
Dr. Loretta Christensen, Chief Medical Officer for the Indian Health Service, spoke to the Medill News Service about what the stamp means for health care community members. “They’re a very unique and special bunch of people that dedicate their lives to caring for others. And so to actually be recognized for that has to be a great moment for them.”
Abortions in South Carolina are banned after six weeks of pregnancy. Local nonprofits are working to help patients anyway
COLUMBIA, S.C. – Between a real estate attorney’s office and a county magistrate building sits one of South Carolina’s three abortion clinics. Pink and white signs beckon patients, discreetly placed so as not to invite unwanted attention.
Since the overturning of Roe v. Wade in 2022, women and advocates in the state of South Carolina have struggled to safeguard access to reproductive health care, including abortions. Existing policies tend to penalize, rather than uplift, patients seeking care and those who help them. But the people who work on the front lines don’t want to leave. Their work is a crucial part of who they are, they say.
South Carolina’s maternal mortality rate is the eighth-highest in the nation, according to the South Carolina Law Review. Vicki Ringer, the director of public affairs at Planned Parenthood South Atlantic, said she is critical of lawmakers focusing on the wrong victims of an under-resourced health care system.
“Women have died and will continue to die,” she said. “This should require some action on behalf of our legislature – whether that’s in research, expanding Medicaid or providing more rural health care. All of those things would make sense, but the legislature does not do any of those things.”
In August 2023, the state Supreme Court upheld a ban on abortion after six weeks of pregnancy, a similar law that had been struck down just eight months before. After the court’s only female justice retired, it reversed this protection, forcing providers to turn away patients at a stage before many of them even know they are pregnant.
While abortion takes center stage as a national political talking point, so many other facets of reproductive care remain difficult to access throughout the country, including contraception, in vitro fertilization and sex education in elementary schools.
“Our reproductive health care restrictions are some of the most restrictive in the nation,” said Kelli Parker, the director of communications and marketing for the Women’s Rights and Empowerment Network (WREN). “Most South Carolinians support access to reproductive health care. But it’s continually being limited through our legislators that have very extreme ideas about what reproductive health care actually is.”

The Planned Parenthood Health Center in Columbia is one of only three abortion clinics in the state of South Carolina. (Simone Garber/MNS)
It never occurred to Parker that her 11-year-old daughter wouldn’t have the same right to bodily autonomy as she once did. Having grown up in New York, Parker’s access to health care in Charleston, S.C. over the past five years has been vastly different from the medical privacy she’s used to.
“I think people who live outside of the South really take for granted the amount of freedom you have,” she said.
Parker’s agency, based in Columbia, works to expand access to health care, education and economic opportunities for women, girls and gender-expansive people throughout the state. Since 2017, WREN has advised patients seeking reproductive services in a state that was one of the first to impose near-total abortion bans after Roe’s reversal.
Recent policing of gender-affirming care comes from male lawmakers’ need for “control,” Parker said.
“It’s important to remember that abortion bans and restrictions don’t do anything to protect anyone’s health or safety – they’re only punishment,” she said. “Why would you want to elect someone who’s out to punish you?”
Ina Seethaler is the director of college outreach at the Palmetto State Abortion Fund, a volunteer-run organization working to offset the financial barriers to reproductive justice in South Carolina. The fund subsidizes abortion procedures and logistical costs, including transportation and lodging for out-of-state appointments.
Seethaler called South Carolina a “reproductive health care desert,” as local physicians often weigh high-stakes decisions that could leave them incarcerated.
According to the S.C. Office for Healthcare Workforce, 14 out of the state’s 46 counties do not have a practicing OB-GYN. That translates to a ratio of 0.43 for every 1,000 women of reproductive age, according to a South Carolina Center for Rural and Primary Healthcare research brief.
“Folks don’t want to move here,” Seethaler said. “They don’t want to practice here. It’s becoming, frankly, kind of dangerous for them to work here. But things are just going to get worse again at the expense of the people in South Carolina.”
And it’s not just a lack of trained professionals that’s driving the reproductive health care shortage. For patients in desperate situations facing few options and little reliable information, many turn to crisis pregnancy centers (CPCs) for answers. These institutions, which reproductive justice advocates say impart misinformation to pregnant people rather than support, generated nearly $1.4 billion in revenue in the 2022 fiscal year and continue to increase in scope and size nationwide.
As a result of CPC expansion, Seethaler said, many reproductive justice organizations are finding it difficult to persuade patients of their legitimacy.
“That overlap is, unfortunately, really problematic,” she said.
The 35 CPCs in South Carolina well outnumber the abortion clinics in the state. In addition to Columbia, two other Planned Parenthood Health Centers are located in Charleston and Greenville, all at least 100 miles away from one another.
Ringer’s lobbying efforts at the Columbia State House are constantly challenged at the clinic sites, where protesters will “literally drag patients into vans” stockpiled with ultrasounds.
“All of these folks exist only to harass patients,” she said. “They don’t provide any real services. It’s just dogma they’re imposing on people that they’re trying to stop from having an abortion.”
These days, the stakes of health care suppression are extending to other reproductive issues. Last month, the Alabama Supreme Court ruled that frozen embryos would be considered “children” under state law, a mandate that could jeopardize the practice of IVF.
While Alabama has since passed a law to protect IVF treatments, legal experts note that language in other states related to so-called fetal personhood leave many open questions about liability.
“Alabama’s ruling is extremely alarming,” Elisabeth Smith, director of state policy at the Center for Reproductive Rights, wrote in a statement. “This is part of the chaos we knew would ensue if Roe v. Wade was overturned. With politicians at the helm instead of doctors, reproductive health care is in crisis.”
Navigating an increasingly polarized workplace and industry, Ringer underscored her personal motivation for continuing this line of work.
“I know that there are others still in this fight, but I can’t just throw up my hands,” she said. “Everybody deserves the right to decide if, when and how to become parents. Pregnant women, most of all, deserve their own freedom to make a decision.”


